I Like That One/Digital Vision via Getty Images
Maggie Ruderman, Boston University and Kimberly Zayhowski, Boston University
Gender reveal parties are best known as celebrations involving pink and blue, cake and confetti, and the occasional wildfire. Along with being social media hits, gender reveals are a testament to how society is squeezing children into one of two predetermined gender boxes before they are even born.
These parties are often based on the 18- to 20-week ultrasound, otherwise known as the anatomy scan. This is the point during fetal development when the genitals are typically observed and the word “boy” or “girl” can be secretly written on a piece of paper and placed into an envelope for the planned reveal.
Now there is a new player in the gender reveal game: genetic screening.
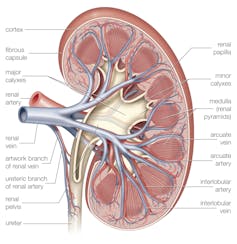
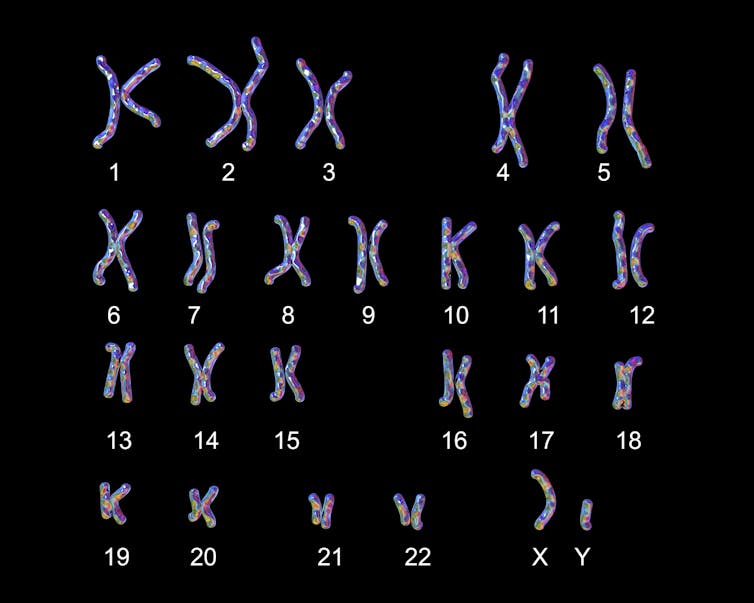
Advancements in genetic research have led to the development of a simple blood test called cell-free DNA prenatal screening that screens for whether a baby has extra or missing pieces of genetic information – chromosomes – as early as 10 weeks into pregnancy. Included in this test are the sex chromosomes, otherwise known as X and Y, that play a role in the development and function of the body.
Anastasia Usenko/iStock via Getty Images Plus
This blood test is more informally called noninvasive prenatal testing, or NIPT. Many people refer to it as “the gender test.” But this blood test cannot determine gender.
As genetic counselors and clinical researchers working to improve genetic services for gender-diverse and intersex people, we emphasize the significance of using precise and accurate language when discussing genetic testing. This is critical for providing affirming counseling to any patient seeking pregnancy-related genetic testing and resisting the erasure of transgender and intersex people in health care.
Distinguishing sex and sex chromosomes
Sex and gender are often used interchangeably, but they represent entirely different concepts.
Typically when people think of sex, they think of the categories female or male. Most commonly, sex is assigned by health care providers at birth based on the genitals they observe on the newborn. Sex may also be assigned based on the X and Y chromosomes found on a genetic test. Commonly, people with XX chromosomes are assigned female at birth, and people with XY chromosomes are assigned male. Since cell-free DNA, or cfDNA, prenatal screening can report on sex chromosomes months before birth, babies are receiving sex assignments much sooner than previously possible.
While cfDNA prenatal screening can offer insights into what sex chromosomes an infant may have, sex determination is much more complicated than just X's and Y's.
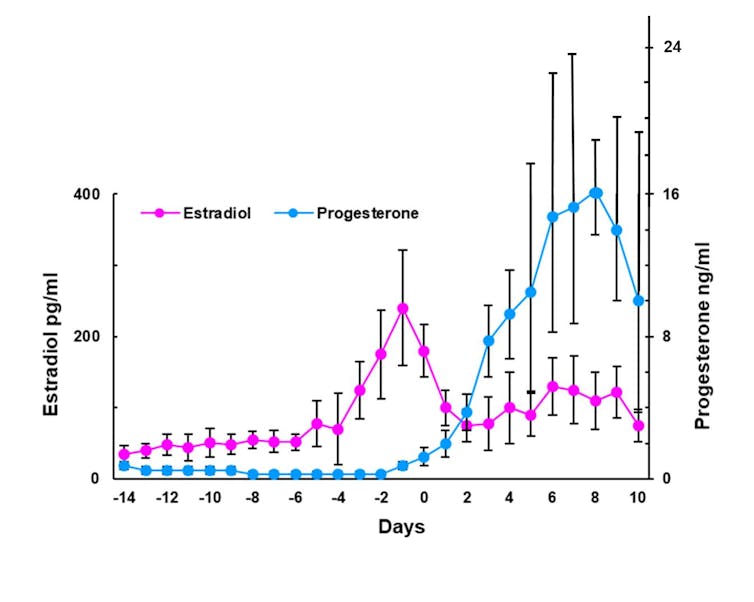
For one, sex chromosomes don't exactly determine someone's sex. Other chromosomes, hormone receptors, neural pathways, reproductive organs and environmental factors contribute to sex determination as well, not unlike an orchestra with its ensemble of instruments. Each cello, flute, tympani and violin plays a crucial role in the performance of the final musical score. There is no single instrument that defines the entirety of the symphony.
Intersex people, or those with variations in sex characteristics that deviate from societal norms of binary sex, exemplify the complexities of sex. These variations can manifest in various ways beyond X and Y chromosomes, such as differences in hormone levels, genitalia or secondary sexual characteristics.
The oversimplification of sex based on societal norms has led many to believe that there are only two discrete sexes. The binary framework of sex excludes intersex people and perpetuates their erasure and mistreatment within both health care and society at large.
For instance, many intersex individuals face unnecessary surgeries, such as nonconsensual genital procedures, to conform to binary norms, violating their bodily autonomy.
Where gender comes in
While sex typically describes someone's anatomical characteristics, gender is an umbrella term that encompasses the way someone views and presents themselves to the world. Countless aspects influence how someone defines their own gender and how the world views their gender, including clothing, haircuts and voice tone. Similar to how Western cultures have historically confined sex to two buckets, it has also created two gender categories: man and woman.
Gender is not dependent on anatomical parts or chromosomes. People are not math equations, and having certain combinations of biological parts does not equal someone's gender. For example, some people may be transgender, meaning their assigned sex is not congruent with their socially or self-defined gender. Nonbinary people do not identify exclusively with either of the two genders in the binary, regardless of their assigned sex.
Just like sex diversity, gender diversity is not rare. A 2022 Pew Research Center analysis found that approximately 5% of adults in the U.S. under the age of 30 are transgender or nonbinary.
These estimates will likely increase as societal awareness and acceptance of gender-diverse individuals increases. Anti-transgender legislation often oversimplifies gender as strictly binary, conflating it solely with sex assigned at birth.
Intersex and gender-diverse people show that sex and gender are both multidimensional. Gender is not solely determined by biology, and it is erroneous to define someone's gender by their sex, much less by their sex chromosomes.
Challenging sex and gender norms
The idea that biology plays the largest role in determining who an individual is, or bioessentialism, has governed misconceptions about sex and gender for many years. This concept is used to confine people to buckets and limit their self-determination.
For instance, societal norms dictate that women should be nurturing and gentle, while men are expected to be protective and assertive. Such rigid gender roles, often enforced through the lens of biology, serve to uphold notions of evolutionary destiny and a purported natural order.

Halfpoint Images/Moment via Getty Images
Marketing strategies for children's toys often adhere strictly to gender roles, steering girls toward dolls and domestic play sets while steering boys toward action figures and construction sets.
Educational systems often reinforce gender norms by directing girls toward subjects such as literature and arts while steering boys toward science and mathematics. This perpetuates the notion that certain traits and interests are inherently linked to one's sex and gender, thereby reinforcing societal norms and sustaining inequality.
Upholding binary constructs of sex and gender does not allow for individuality and gender fluidity. Categorizing people from the time their chromosomes are analyzed or the moment their genitals are observed at birth restricts their autonomy and authenticity. These simple assumptions set expectations that can be harmful.
Letting children define themselves
If you're a parent offered cfDNA prenatal screening during pregnancy, remember that it is commenting only on one instrument in the orchestra of sex. It cannot examine all of the other factors that determine sex as a whole. And it most certainly cannot determine gender, which is an entirely different concert.
In recent years, Jenna Karvunidis, the mother considered the inventor of gender reveal parties, shared her regrets for starting the trend and noted that her views on sex and gender have shifted. In a 2019 Facebook post, Karvunidis wrote, “PLOT TWIST. The world's first gender reveal party baby is a girl who wears suits!” She had also gone on to say, “Celebrate the baby … Let's just have a cake.”
When the envelope is opened, the balloons are popped and the crafty cake is cut, consider how these practices perpetuate social confinements and a gendered destiny for your little bundle of joy. Perhaps opt simply for a celebration that leaves space for your child to one day define who they are.
Maggie Ruderman, Assistant Professor of Medicine, Boston University and Kimberly Zayhowski, Assistant Professor, Boston University
This article is republished from The Conversation under a Creative Commons license. Read the original article.